GPs' identification of patients with mental distress: a coupled questionnaire and cohort study from norwegian urban general practice, BMC Primary Care
By A Mystery Man Writer
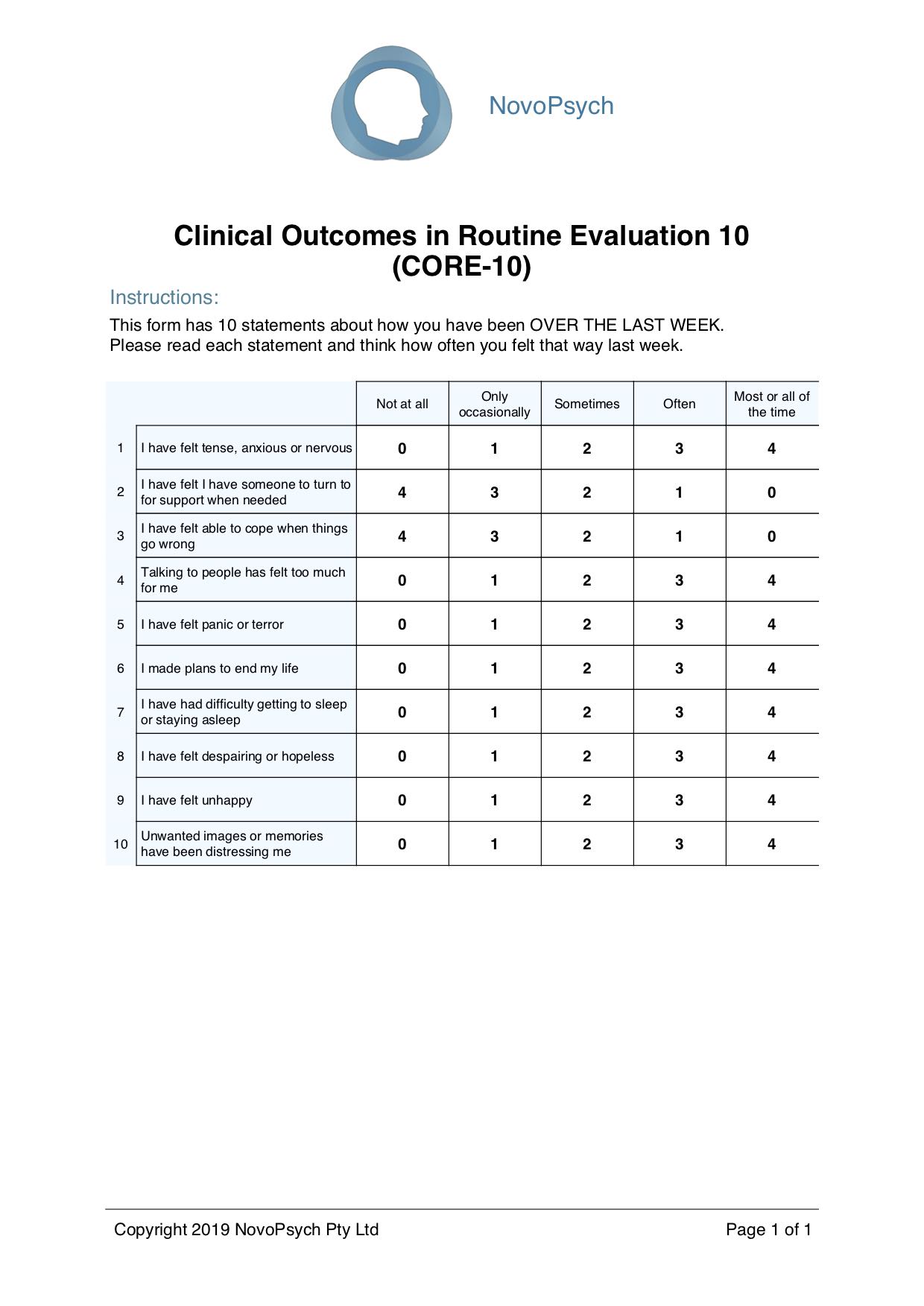
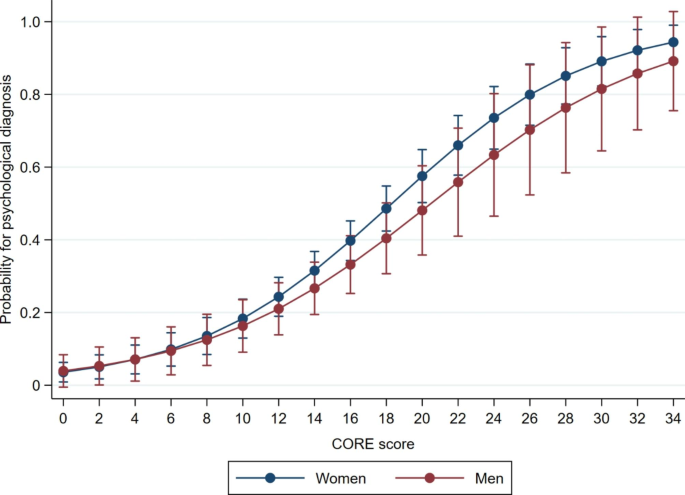
Background Mental health problems are one of the leading causes of disease burden worldwide, and are mainly diagnosed and treated in general practice. It is unclear however, how general practitioners (GPs) identify mental health problems in their patients. The aim of this study was to explore how patients’ self-reported levels of mental distress correspond with psychological diagnoses made by their GPs, and associations with sex, age, number of consultations, and somatic symptom diagnoses. Methods A questionnaire study coupled with retrospective and prospective cohort data from 553 patients aged 16–65 years in six GP offices in Oslo, Norway during 21 months in 2014–2016. Results We found that 73.3% of patients with self-reported high levels of mental distress versus only 13.3% of the patients with low levels of mental distress had received a psychological diagnosis (p < 0.01). We found an increase in number of consultations for the group with high levels of mental distress regardless of having received a psychological diagnosis (p < 0.01). There was also an increase in number of somatic symptoms (p = 0.04) and higher number of females (0.04) in this group. 35% of patients had received one or more psychological diagnosis by their GP. Mean CORE-10 score, being female and a high number of consultations was associated with having received a psychological diagnosis. In the adjusted analyses high CORE-10 score and a high number of consultations still predicted a psychological diagnosis. Conclusions We found a clear association between self-reported mental distress and having received a psychological diagnosis amongst the participants, and the probability for being identified increased with increasing levels of mental distress, and increasing number of visits to their doctor. This suggests that GPs can identify patients with high levels of mental distress in general practice in an adequate way, even though this can sometimes be a complex issue. Trial registration Trial registration The main study was retrospectively registered in ClinicalTrials.gov on August 10 2019 with identification number NCT03624829.
Diabetes Canada Clinical Practice Guidelines

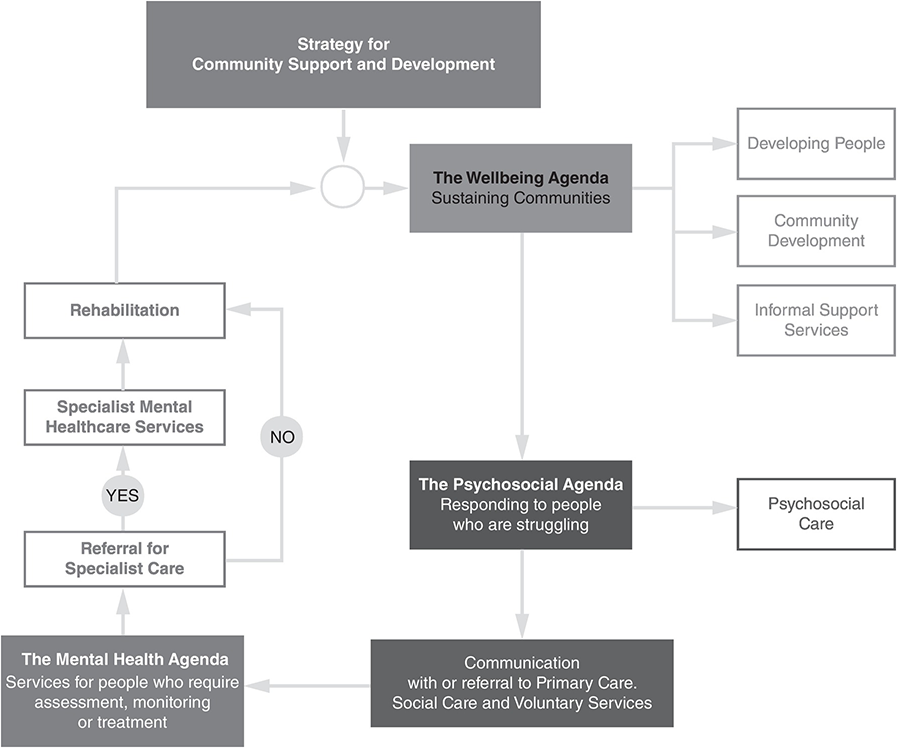
Implementing Mental Health Promotion in Primary Care
August 2023 – Michael Tam
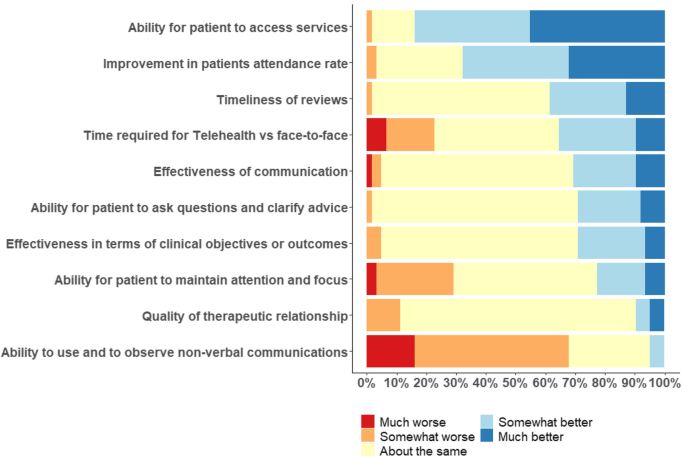
Mental health professionals and telehealth in a rural setting: a cross sectional survey, BMC Health Services Research
The Nature and Impacts of Twenty-First-Century Healthcare Emergencies (Section 1) - Major Incidents, Pandemics and Mental Health
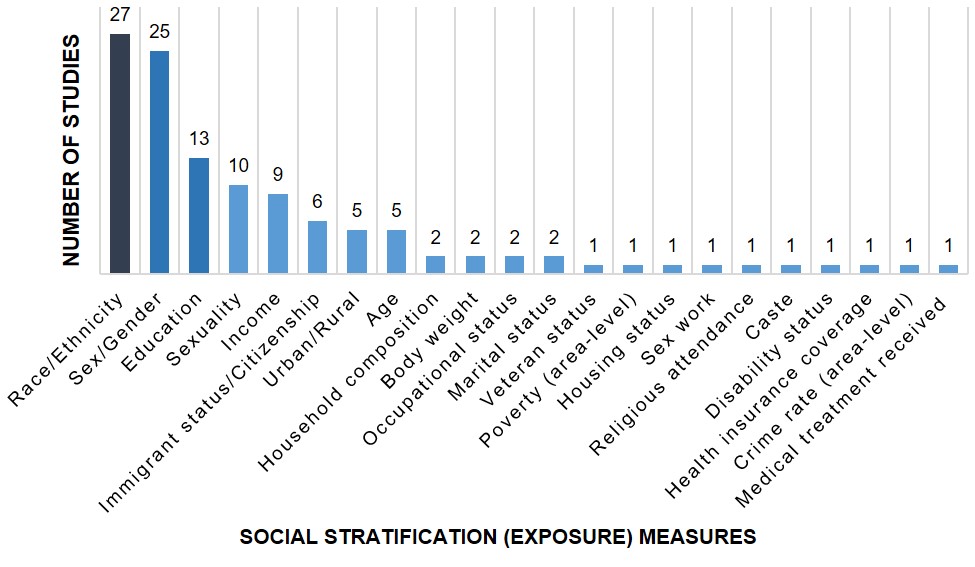
How to integrate Intersectionality Theory in Health Equity analysis

Care providers' experiences with and attitudes towards virtual antenatal care: Findings from a qualitative study in British Columbia - Jude Kornelsen, Daria Nowaczek, Robin Johnson, Mona Mattei, Shiraz Moola, 2022
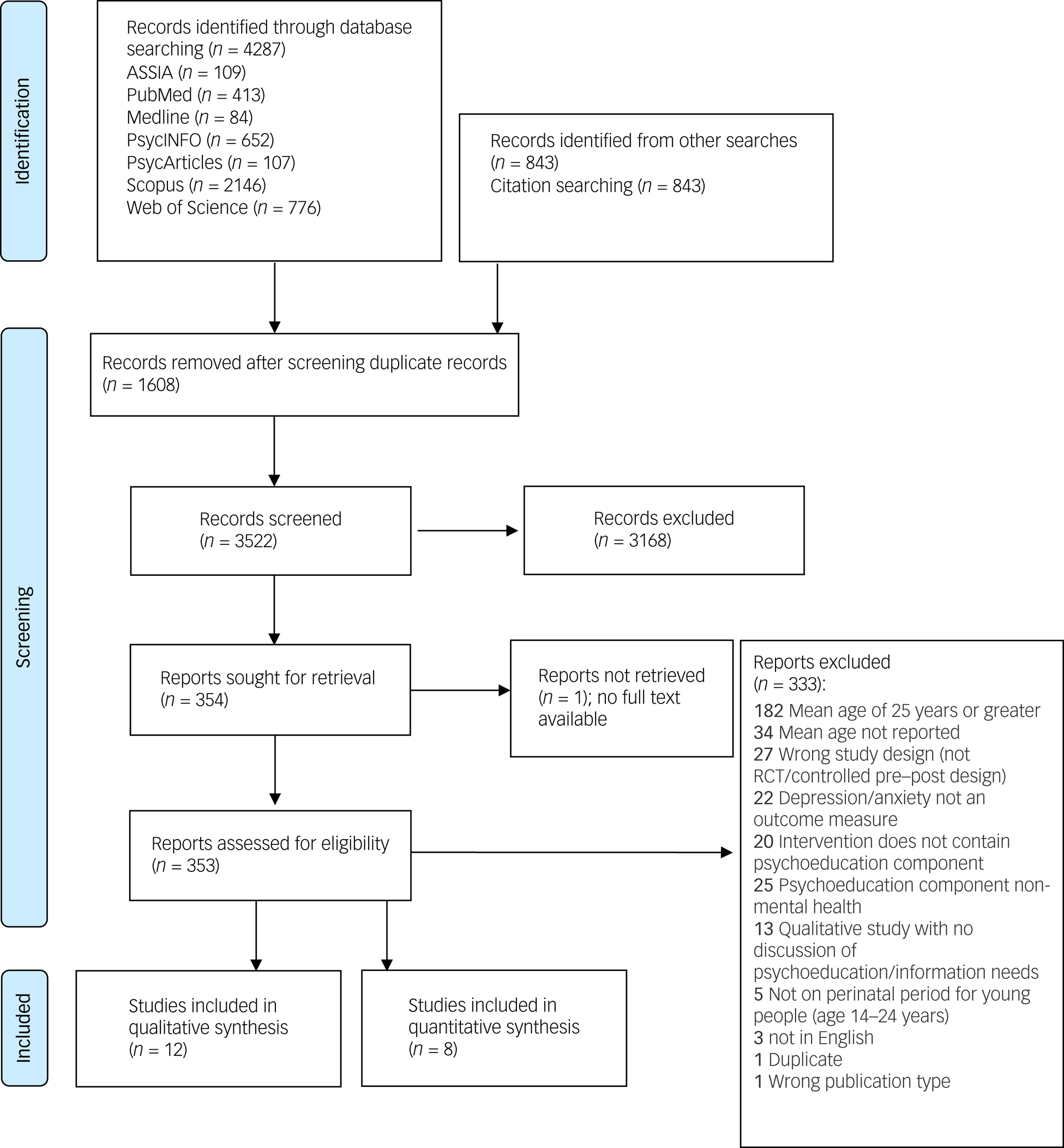
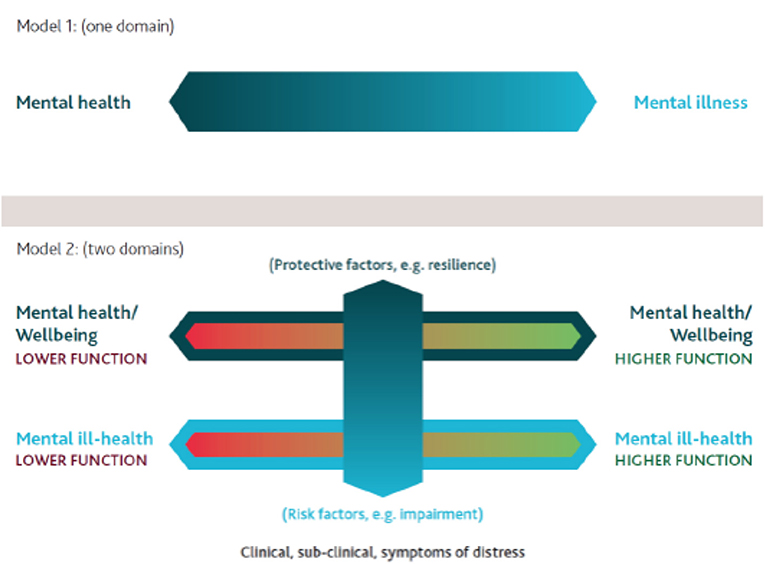
Psychoeducation as an active ingredient for interventions for perinatal depression and anxiety in youth: a mixed-method systematic literature review and lived experience synthesis, BJPsych Open

GP preferences for, access to, and use of evidence in clinical practice: a mixed-methods study
Frontiers A Public Mental Health Study Among Iraqi Refugees in Sweden: Social Determinants, Resilience, Gender, and Cultural Context

General practitioner strategies for managing patients with multimorbidity: a systematic review and thematic synthesis of qualitative research, BMC Primary Care

Nature Contact and Human Health: A Research Agenda, Environmental Health Perspectives
- Fantasie Women's Lois Underwire Side Support Bra, Black, 32HH : : Clothing, Shoes & Accessories

- Drawstring Linen Pants Women Korean Womens Linen Trousers - Casual 100% Linen - Aliexpress

- Sonryse 053ZL Fajas Colombianas Moldeadoras Postparto y Postoperatorias Sonryse SON-053ZL

- Wonderbra Ultimate Silhouette Strapless bra DD-G cup SKIN –

- Making angel wings 👼🏻 DIY